Table of Contents
Fungal Acne – Explanation
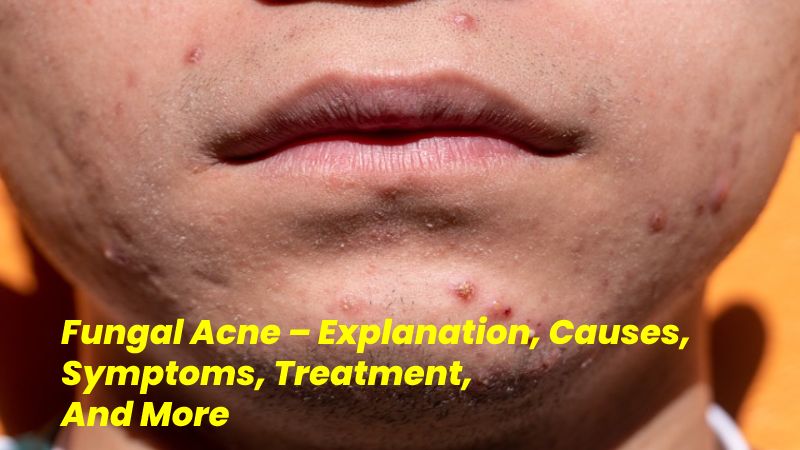
Fungal acne is a type of pollution in your skin’s hair glands. It most normally appears as small pimples that don’t vary much in shape or size, often along with itching. Fungal acne can cause whiteheads and skin annoyance. It’s often disorderly for acne vulgaris. This is the type of acne most usually related to blackheads and whiteheads.
If you save using anti-acne treatments, you can brand fungal acne inferior. But fungal spots and acne vulgaris are two different situations caused by two other things. They won’t reply to the same treatment. That’s why it’s essential to understand what fungal acne looks like and how it produces. Read on to learn the indications and signs of fungal acne and what you can do to treat and stop breakouts.
If I have Fungal Acne
In contrast, there are closed comedowns, open comedowns (blackheads), nodules, cysts, and abscesses in usual acne. Spots can be of varying sizes too. You should start treating the blemished skin early on as well, to prevent most damage.
- Forehead, temples and frontal hairline
- Upper chest
- Upper and mid-back
In contrast, there are closed comedowns, open comedowns (blackheads), nodules, cysts, and abscesses in usual acne. Spots can be of varying sizes too.
Causes of Fungal Acne
Fungal Acne is a While of a Misnomer. Unlike acne, fungal acne isn’t caused chiefly by oil and bacteria in pores. However, oil and sebum production is a big part of helping feed the germs that cause fungal acne.
Instead, the pimple-like knocks and irritated skin associated with fungal acne are caused by an overgrowth of yeast, a type of fungus. That’s why it’s occasionally called fungal acne. It’s also mentioned to as Pittosporum folliculitis or Malassezia folliculitis.
Some of Causes and Deterrence
There are a few motives you may be receiving fungal acne. Here’s come again they are and how you can mitigate them.
- Heat and Humidity: Fungal acne is carefully related to warmer weather. According to Eichner, it’s relatively uncommon in the United States and is seen at much higher rates in areas of the world where the weather is always warm, such as the Philippines. The mushroom that causes fungal acne thrives in moist environments with excessive sweat and heat.
- Sweat: You maybe already know that it’s best to shower as soon as your exercise is over and that it’s not ideal to sit around in sweaty, clingy clothes, but this can do more than make for an uncomfortable fit. To avoid sweat-induced fungal acne, Sham ban advises to “Select loose clothing with natural fabrics, avoid spandex, and change clothing often after exercise or extreme sweating. This can be helpful, mainly in hot weather when it can flare up.”
- Overuse of antibiotics: The moulds on our skin are part of our microbiome, and they’re not a problem when they’re not in excess. However, “in certain circumstances—such as continuing use of topical and oral acne antibiotics—the normal skin flora is wiped out by the antibiotics, and so the yeast flourishes, causing inflammation and Rabbah describes. If you have acne that’s not replying to standard actions and a past of regular antibiotic use, you may have found your offender.
- Contact with Others: Might be transmittable. If you’ve had a physical connection with someone who has it may be your cause of yours.
Natural Balance
The yeast responsible for is constantly current on your skin. Typically, your body can balance the mould, different fungi, and bacteria that are also a part of your skin.
But if that natural balance is upset, an overgrowth can happen. That’s when the infection of hair glands develops, and acne-like symptoms display up.
Many conditions or Events Can Upset this Stability of Bacteria and Fungi, With:
- Trapped moisture. Wearing clammy workout clothes for too long can inspire yeast growth. Reweaving test clothes without washing them may also expose your skin to fungi that have grown in the clothes.
- If you take antibiotics, the bacteria on your skin can be reduced. That can let aimed at the overgrowth of a fungus—the suppressed resistant system. People with cooperated immune systems may be more likely to grow fungal acne.
- Diet vagaries. Fungi and mould food on carbohydrates, so opposite your consumption of sweets and carb-rich foods may help sluggish fungal growth.
- She was trying on tight clothes. Regularly trying nonbreathable clothes can encourage extra sweat and moisture. This can foster a skin situation ripe for yeast growth.
- Sincere, moist environments. People in hot climates, where sweating is more likely, may frequently experience it.
The Symptoms
One of the motives that can last for so long is because looks like Vulgaris or bacterial acne. Not knowing the difference, people may treat it with regular skincare options. These actions don’t work, making the infection not as good.
Here’s In what way to Tell the Difference Between an Infectious
- Infectious acne can cause pimples and whiteheads of varying sizes—pus-filled knocks caused by an incline to be closely the same size.
- Repeatedly shows up on the weapons, chest, and back. It can also be on the face, anywhere most common bacterial acne.
- Often causes itchiness. Bacterial acne rarely does.
- Fungal acne often appears in collections of tiny whiteheads. Bacterial acne is less clustered and sparser. Results from yeast growth, so you may experience other yeast-related conditions, like psoriasis and dandruff. This can help determine whether your breakouts are from yeast or another cause.
Some of the Treatment
Fungal acne is often treated unsuitably because it looks regular. Many people use common anti-acne treatments against it, but those won’t work. To properly treat the fungal infection, you need to return the skin’s balance between yeast and bacteria. Several treatment options can help do this.
Fungal acne isn’t solid to treat—once you know, that’s what you’re commerce with. The challenge is that can look similar to regular. In short, the illness we call results from an overgrowth of yeast. “Otherwise known as pittosporum folliculitis”, according to board-certified dermatologist Morgan Abacha.
To set the record traditional: fungal acne is a total contradiction—”it has nothing to do with fungus, nor is it acne—it’s a folliculitis, or infection of the tiny hair follicles on the face or body,” which leads to “papules, small, raised, solid bumps resembling pimples.
Here are some more critical points about fungal acne:
Cause: The main culprit behind fungal acne is the giantism of the yeast Malassezia on the skin. This yeast is commonly found on the skin’s surface, but when it multiplies excessively, it can lead to inflammation and acne-like eruptions.
Symptoms: Fungal acne often appears as small, uniform red, or skin-colored bumps that may be itchy or tender. It typically occurs on the chest, back, shoulders, and forehead – areas with more sebaceous (oil-producing) glands.
Shower More Frequently
If you often work out or have a job that reasons you to sweat, try showering and altering garments right after the gym or work. This can help wash away excess yeast that may have ongoing rising in the warm, moist environments that grow in sticky clothes.
Wear Looser Clothes
If you regularly wear tight clothes, friction and low airflow can inspire yeast development on the skin. Opt for loose, breathable fabrics more often to help your skin get a proper flow and encourage balanced bacterial and fungal growth.
Conclusion
Fungal acne is an infection in hair follicles caused by an overgrowth of yeast. Despite the name, it’s not like the acne that causes whiteheads and blackheads. Typical anti treatments won’t work for Instead, you need to identify this type of infection to treat it accurately.
Learning how to identify this specific type of skin infection can also help you prevent future.
Also Read: Green Tea -Information, Benefits, Different, And More